In 2024 the Bureau established an Independent Health Care Provider Assistance Program, pursuant to 24-A M.R.S. § 4329. This program provides assistance to independent health care practitioners who have questions or complaints regarding their dealings with insurance carriers. The program answers questions from these providers and investigates filed complaints. The program does not assist with issues regarding contract negotiations between providers and insurers.
The law requires the Bureau to annually publish aggregate data regarding complaints on its webpage.
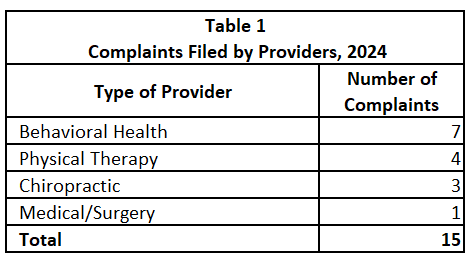
The following tables contain aggregate information from complaints received between August 9, 2024 (when the law went into effect) and December 31, 2024.
Provider complaints compiled in Table 1 included the following issues: contractual issues (including coding and prepayment audits), unpaid self-funded claims that are not subject to the Maine Insurance Code, credentialing, and out-of-network (OON) services.
In 2024, the Bureau facilitated one recovery of $1,077.74.
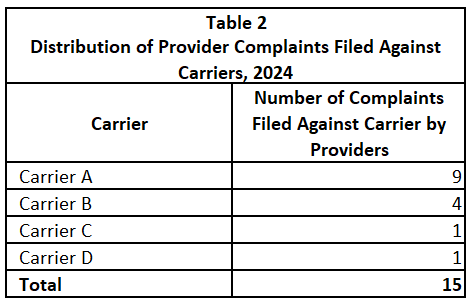
As shown in Table 2, 9 of the 15 total provider complaints in Table 1 were filed against the same carrier.
In addition to the 15 complaints, the Bureau assisted with 53 inquiries from providers during this time period. Questions from providers included clarification about which issues are and are not within the Bureau’s jurisdiction, and requests for assistance with finding various types of information on the Bureau's website.