In this issue:
- Mandated CME Audits
- Mandated Opioid CME
- Physician Assistant Questions About CME
- Changes in Physician Assistant Licensure
FROM THE CHAIR
Diversity, Equity and Inclusion
Maroulla S. Gleaton, M.D., Chair
Introduction
I recently have been elected to serve on Board of the Federation of State Medical Boards. This is a 3-year position. At my first Board meeting we discussed two major issues affecting state member boards. The first being Diversity, Equity, and Inclusion and the second being the effect of the recent Supreme Court decision in Dobbs v. Jackson Women’s Health Organization that changed the federal protection rights for women by enabling each state to legislate women’s rights. I would like to cover both issues starting with the topic of Diversity, Equity, and Inclusion and deferring the abortion topic for my next newsletter article.
Diversity, Equity, and Inclusion
Many studies have shown that racial inequities are a major public health concern in the US. The majority of physicians, especially medical students and residents, feel that patients get differing levels of medical treatment based on race, according to the recently interviewed board chair of the American Academy of Family physicians, Ada Stewart, MD. Furthermore, more than three quarters of physicians feel that this type of inequity needs to be addressed.
The FSMB has formed a workgroup to examine this topic and make recommendations. Jeff Carter, MD, an anesthesiologist from Missouri, is chair elect for the FSMB and chair of the workgroup on Diversity, Equity, and Inclusion in Medical Regulation and Medical Care. I would like to give some history and background concerning discrimination and then move on to the ideas put forward by the workgroup, and end with comments on our own medical board and the physicians of this state.
There has been a history of public acknowledgement of inequity in medical practice in the US starting with President Reagan who highlighted incidents in America’s history that he wanted to apologize for such as the US role in shielding Nazi war criminals and the CDC’s notorious Tuskegee medical experiment. The FSMB can look back at its own history: bias against “irregular physicians” who were osteopathic physicians, or discrimination against IMG (international medical graduates) physicians calling those physicians an “invasion of undesirables” when they applied for medical licensure in the different states, and clearly for many, many years there was failure to seek out women and people of color for governance positions in the FSMB. The FSMB did not create all these biases but certainly perpetuated them.
In recognizing and being transparent about the inappropriateness of this behavior the FSMB issued the following statement: “We acknowledge our role in a system that has allowed racist, biased, and inequitable influences to hinder . . . safety and harm patients and we commit to identifying, addressing and dismantling those influences.” The workgroup among other things hopes to identify best practices to share with member state boards for insuring fairness in board decision making related to licensing and disciplinary actions. Its final report is to come out in spring 2023.
As a next step to continue to highlight and make reparation regarding this issue there will be a peer reviewed article released in the Journal of Medical Regulation over the next 6-8 months. The Maine Medical Association also has recently formed an ad hoc committee charged with examining this issue in our state and made this the major topic at its annual session in September 2022.
For our Maine Board of Licensure in Medicine we, along with many others in the country, have noted that the issue of medical practice inequality was especially highlighted during the COVID pandemic when disadvantaged minority populations clearly experienced the brunt of unfortunate medical outcomes. It will take time to examine the whys to get to the heart of next steps to reduce inequalities. We are making progress in recognizing these issues and concerns and will be crafting new ways to achieve meaningful diversity, equity, and inclusion.
WHAT EVERYONE SHOULD KNOW
Watch How the Board Works
The Board has created 3 short (30 second) videos describing the Board and it functions. The videos can be found on our website at https://www.maine.gov/md/about and https://www.maine.gov/md/complaint/file-complaint.
The three videos include:
- An Introduction to the Board;
- An Introduction to the Complaint Process; and
- Grounds for Discipline (What the Board can and cannot investigate).
The Board plans to produce additional related videos including:
- Licensing
- The process for obtaining an initial license;
- The process for renewing a license;
- The process for taking the online Jurisprudence exam.
- Complaints and Investigations
- Step by step instructions for filing a complaint.
Feedback regarding the videos can be sent to Assistant Executive Director, Tim Terranova at tim.e.terranova@maine.gov.
Did You Know - You Can Observe Board Meetings Online
The Board holds regular meetings every second Tuesday of the month. The meetings have primarily been virtual during the previous twenty-four months and available for public observation via the platform Zoom. Licensees who are interested in learning more about the Board’s processes and procedures regarding licensure, complaints, investigations, and rule- making are encouraged to “Zoom into” one of the Board meetings to watch and listen. Doing so will de-mystify questions regarding the Board, its members, and the way in which it goes about its statutory mission to protect the public. Information regarding the dates of the monthly Board meetings and the Zoom information to access the meeting are available on the Board’s website: https://www.maine.gov/md/about/board-meetings-minutes. Check it out!
A CASE TO CONSIDER
A case to Consider
The Board includes summaries of adverse actions in its periodic newsletters as a means of educating licenses regarding the issues that can lead to discipline. One of the issues that can lead to discipline is a violation of clinician-patient boundaries. Appropriate clinician-patient boundaries are required by applicable codes of ethics and standards, and by Board rule Chapter 10, which prohibits clinician sexual misconduct. Despite the existence of these ethical codes and rule, the Board continues to encounter instances of clinician-patient boundary violations. The following is an excerpt from an actual case concerning this issue:
THE CASE
A female patient complains that following a brief initial office visit, the physician showed up at her place of employment the next day telling her that he thinks she is beautiful, which made her uncomfortable. Two days later she received a letter from the physician at her home stating, among other things that made her feel uncomfortable, that he rarely felt so attracted to someone. This letter was followed by the physician leaving gifts (including his book and flowers) at her place of employment and admitting to the patient that in order to send her the letter he had obtained her home address from her medical chart. When the patient asked if this was legal, he told her, “Well yes, I make house calls. I’m a doctor.”
The physician replies that the patient misinterpreted his intention merely to be friendly and establish a good relationship with a new patient. He thinks being “too professional,” can seem unfriendly, or uncaring, and can be counterproductive.
How many boundary violations can you see in this actual case?
- Using information gained during the patient encounter/patient’s medical record regarding the patient’s place of employment and residence
- Showing up at the patient’s place of employment the next day for the purpose of soliciting a personnel relationship
- Telling the patient that she is beautiful
- Sending the patient a letter to her place of residence soliciting a personal relationship
- Leaving gifts and flowers for the patient at her place of employment in an effort to solicit a personal relationship
- Telling the patient that he “makes house calls” as a cover for accessing the patient’s home address – so that he could send her a letter soliciting a personal relationship
There are four potential statutory grounds for discipline based upon the above conduct:
- Pursuant to 32 M.R.S. § 3282-A(2)(C), the Board may impose discipline for a professional diagnosis of a mental or physical condition that has resulted or may result in the licensee performing services in a manner that endangers the health or safety of patients.
- Pursuant to 32 M.R.S. § 3282-A(2)(E), the Board may impose discipline for engaging in conduct that evidences a lack of ability or fitness to discharge the duty owed by the license to a patient or the general public, or that evidences a lack of knowledge or inability to apply principles or skills to carry out the practice for which the licensee is licensed.
- Pursuant to 32 M.R.S. § 3282-A(2)(F), the Board may impose discipline for unprofessional conduct for engaging in conduct that violates a standard of professional behavior that has been established for the practice of medicine.
- Pursuant to 32 M.R.S. § 3282-A(2)(H), the Board may impose discipline for violation of Board statute or rule, including violation of Board Rules Chapter 10 Sexual Misconduct for sexual impropriety by using the physician-patient relationship to solicit or initiate a date or sexual or romantic relationship.
Maintaining appropriate clinician-patient boundaries is critical to the health and welfare of the patient, whose interests should be paramount. The clinician-patient relationship is inherently unequal and patients rely upon clinicians to only act in their best interests. Violation of patient privacy and their confidential health care information in order to solicit a personal relationship is unethical, unprofessional, and harms patients.
The Board hopes that you reflect upon this actual case and the importance of maintaining appropriate clinician-patient boundaries.
ADVERSE ACTIONS
Adverse Actions
In 2021 the Board reviewed 305 complaints and investigative reports – an average of 25 per meeting. While the number of complaints received by the Board remains consistently large, the number of complaints that result in adverse action is quite small. In most cases, the conduct resulting in adverse action is egregious or repeated or both.
The Board’s complaint process is relatively straight-forward. FAQs about the complaint process are available on the Board’s website: https://www.maine.gov/md/complaint/discipline-faq. Brochures regarding the complaint process are also available on the Board’s website: https://www.maine.gov/md/resources/forms.
Upon receipt of a complaint, it is forwarded to the licensee for a written response and a copy of the medical records. In general, the licensee’s response is shared with the complainant, who may submit a reply. The Board reviews the complaint file once completed, and may take any of the following actions:
- Dismiss
- Dismiss and issue a letter of guidance
- Further investigate
- Invite the licensee to an informal conference
- Schedule an adjudicatory hearing
The following adverse actions are being reported for the purpose of educating licensees regarding ethical and/or legal issues that can lead to discipline, and to inform licensees of any limitations or restrictions imposed upon scope of practice.
Elmer H. Lommler M.D. License #MD9862 (Date of Action 06/16/2022)
Effective June 16, 2022, the Maine Board of Licensure in Medicine ("Board") stayed the September 15, 2021 suspension of Dr. Lommler's license to practice medicine imposed for noncompliance with the March 12, 2021 Decision and Order.
Elmer H. Lommler M.D. License #MD9862 (Date of Action 06/15/2022)
On June 15, 2022, the Board issued a decision and order on Dr. Lommler's appeal of the preliminary denial of his license renewal. The Board found that Dr. Lommler failed to comply with several provisions of the Board's March 12, 2021 Decision and Order and imposed a ten-year probation with the following conditions: a) Dr. Lommler must engage in counseling with a psychologist and have his medications managed by a psychiatrist with reports to be submitted to the Board; b) Dr. Lommler's practice is limited to four days a week; c) Dr. Lommler must establish a colleague to be available when he is not present if his office is open; d) Dr. Lommler must have a Board approved physician practice monitor working in his office at least one day a week who will submit reports to the Board; e) Dr. Lommler must share call with two other providers proportionate to the providers' full-time equivalent time in the practice; and f) Dr. Lommler may not provide medical care to his employees. In addition, the suspension imposed in accordance with the March 12, 2021 Decision and Order was stayed and Dr. Lommler’s renewal application was granted.
Marc DeBell, M.D. License #20244 (Date of Action 06/14/2022)
On June 14, 2022, Dr. DeBell entered into a First Amendment to Consent Agreement with the Board which granted Dr. DeBell's application to convert from inactive to active status, imposed a warning for his failure to comply with all terms of the June 12, 2019 Consent Agreement, required that he comply with all provisions of the reentry to practice plan submitted to the Board that includes a Preceptor submitting reports to the Board, and imposed a requirement that he maintain enrollment in and comply with a monitoring agreement with the Maine Professionals Health Program (MPHP) for a period of not less than five years.
Morris S. Minton, Jr., M.D. License #MDE21968 (Date of Action 05/10/2022)
On May 10, 2022, the Board determined that Dr. Minton allowed his license to expire while under investigation for allegations relating to unprofessional conduct.
David R. Austin, M.D. License #MD12687 (Date of Action 4/12/22)
On April 12, 2022, the Board voted to accept Dr. Austin's request to permanently surrender his license while under investigation for allegations of substance misuse and unprofessional conduct.
Kristin H. Coleman, M.D. License #MD15593 (Date of Action 3/23/22)
On March 23, 2022, Kristin H. Coleman, M.D. and the Board entered into a Consent Agreement for Conversion to Active Status. Dr. Coleman last practiced clinical medicine in 2008. The consent agreement incorporates a reentry to practice plan that includes completion of a reentry program, a physician mentor/preceptor who will provide reports to the Board, and a period of observation/supervision and review of clinical care.
LICENSING ISSUES
Mandated CME Audits
A Board rule requires Board staff to complete random audits of CME during the renewal process. The audits were placed on hold at the beginning of the pandemic, starting in March 2020. The audit process has now been reinstated.
What does this mean? 10% of renewal applicants are randomly selected each month. If selected, the applicant is notified at the time of their renewal and, in addition to reporting their CME, they must provide proof of its completion. Proof can include copies of certificates or a CME log provided by a professional organization. A self-made spreadsheet with courses listed is not acceptable.
How much CME do I need to show? Physician licensees need to provide proof of 40 AMA Category 1 CME, including 3 hours of AMA Category 1 opioid related CME. Physician assistant licensees need to show proof of either current NCCPA certification or 50 AMA Category 1 CME. In addition, physician assistant licensees need to show proof of 3 hours of AMA Category 1 opioid related CME. Please note that physician assistants who are not NCCPA certified need to earn 50 AMA Category 1 CME and 50 AMA Category 2 CME each renewal cycle, but Category 2 CME is not audited.
How do I provide the proof? If you have the proof available as a PDF when submitting your renewal application, you have the option to upload it at that time. Otherwise, you can e-mail the proof to medicine.pfr@maine.gov.
What happens if I have trouble finding the proof of completion? Licensees selected for audit will not be renewed until the proof has been submitted and verified. Failure to provide the proof in a timely manner will result in the application being referred to the full Board for possible action.
Is there a better way of doing this? Yes, the Accreditation Council for Continuing Medical Education (ACCME) is the national entity which accredits organizations that provide continuing medical education. ACCME has created the “Program and Activity Reporting System (PARS)” which allows accredited CME providers to input the information regarding CME participants and activities into a secure database. The Board has access to PARS and when a licensee is randomly selected for an audit, Board staff proactively check PARS to see if enough CME has been reported. If the CME is found, the licensee is never notified of the audit, but it is listed as passed in their licensure file. In addition, there is no delay in processing the renewal. Reporting CME credit to PARS is voluntary and not all accredited CME providers are currently doing it. When you sign up to participate in a CME activity, you can ask the CME provider if they report your CME credit in PARS. If they have questions about how to do that, they can contact the ACCME at info@accme.org.
What if I have questions? Please contact one of our licensing specialists.
Tracy Morrison
Licensure Specialist (207) 287-3602
tracy.a.morrison@maine.gov
Last Name A-L
Lisa Reny
Licensure Specialist (207) 287-3782
lisa.m.reny@maine.gov
Last Name M-Z
Mandated Opioid CME
When it is time to renew your license there are several items that can cause a delay. One of the most common items is the failure to obtain 3 hours of opioid CME every two years.
Board Rule Chapter 21 states:
By December 31, 2017, and thereafter, clinicians must complete 3 hours of Category 1 credit Continuing Medical Education (CME) every two years on the prescribing of opioid medication as a condition of prescribing opioid medication. By December 31, 2018, and thereafter, all clinicians must complete 3 hours of Category 1 credit Continuing Medical Education every two years on the prescribing of opioid medication regardless of whether or not they prescribe opioid medication.
The full rule can be found at https://www.maine.gov/md/sites/maine.gov.md/files/inline-files/Chapter%2021%2005.27.20.pdf.
Every month there are 10 to 15 licensees who indicate they have not obtained the CME on their renewal application. This causes the application to be pended and, if it goes past the expiration date, requires the licensee to explain to their employer and every insurance company why their license has not been renewed.
Every licensee must obtain 3 hours of opioid related CME every two years. There are good reasons for this rule. We are in the middle of an opioid epidemic and, whether or not you prescribe these medications, as an active clinician you come into contact with patients who are or have been affected by opioids. Whether or not you prescribe them, it is your duty to understand how they affect the patient you may be treating and/or interact with medications you may be prescribing. We often receive complaints, especially from radiologists and pathologists that they don’t interact with patients and should be exempt. However, over the years the Board has seen clinicians in both specialties who have prescribed these medications for patients, families, or friends.
Unlike other states, the Board does not require a specific course. You can choose what opioid related course(s) to take. However, in order to help licensees meet this requirement, the Board has worked with Maine Medical Association Center for Quality Improvement to provide free opioid related CME. The CME is online and available any time at https://qclearninglab.org/all-courses/, The CME is reviewed and updated on a regular basis.
Please be aware of your requirements for licensure and take advantage of the resources provided by the Board.
Physician Assistant Questions About CME
Physician Assistant licensees often have questions about their CME at the time of renewal. The most often reiterated concern is that the cycle for CME certification through the National Commission on Certification of Physician Assistants (NCCPA) is not complete.
The NCCPA is a private organization that certifies physician assistants through examinations. The NCCPA does NOT grant you a license to render medical services in the state of Maine. You are responsible for following the rules and regulations of Maine if you wish to maintain your licensure in the state.
In Maine, NCCPA certification is required for initial licensure, but is not required to maintain your license. However, if you maintain your NCCPA certification you are deemed to have met all the CME requirements for renewal except for the additional requirement of 3 hours of AMA category 1 opioid related CME.
So, if you are currently NCCPA certified you can answer yes to the questions, “Have you earned the 50 CME Category I credits required or are you currently NCCPA certified?” and “Have you earned the total of 100 CME Category I and Category II credits required or are you currently NCCPA certified?” You will not need to provide or list the CME you have completed.
If you have questions, please contact one of our licensing specialists.
Tracy Morrison
Licensure Specialist (207) 287-3602
tracy.a.morrison@maine.gov
Last Name A-L
Lisa Reny
Licensure Specialist (207) 287-3782
lisa.m.reny@maine.gov
Last Name M-Z
Changes in Physician Assistant Licensure
LD 1660 was enacted as emergency legislation in March, 2020, and made several changes to Physician Assistant (PA) licensure. Many of those changes were waived during the declared state of emergency in Maine, which ended on June 30, 2021.
During that time, the Board of Medicine and the Board of Osteopathic Licensure worked to implement new rules, conforming to the new law, and update their technical systems to match the new requirements. The new rule, htthttps://www.maine.gov/md/sites/maine.gov.md/files/inline-files/Chapter%202%20effective12.16.20.pdf, was enacted on December 16, 2020 and the technical changes went live on January 6, 2021. Since that time Board staff have worked to educate PAs and systems that employee physician assistants about the changes. Unfortunately, a year and a half after the rule went into effect, and a year after the end of the declared emergency, there appears to be continued confusion regarding the requirements.
In general, physician assistants are broken into two groups, those with fewer than 4,000 clinical hours since graduation and those with more than 4,000 hours since graduation.
If a physician assistant has fewer than 4,000 clinical hours they must submit either a uniform notice of employment or a collaborative practice agreement before they can provide medical services in Maine.
A scope of practice agreement or, uniform notice of employment, https://www.maine.gov/md/sites/maine.gov.md/files/inline-files/Uniform%20Notification%20Form_2.pdf is used when the physician assistant works in a health care system or physician group practice that has a system of privileging and credentialing.
A collaborative agreement, https://www.maine.gov/md/sites/maine.gov.md/files/inline-files/Uniform%20Collaboration%20Practice%20Agreement%20Application%20Review%20Form_0.pdf, is required when the physician assistant works in a setting that is not a health care system or physician group practice as defined above.
Physician assistants with more than 4,000 clinical hours need a practice agreement, https://www.maine.gov/md/sites/maine.gov.md/files/inline-files/Uniform%20Collaboration%20Practice%20Agreement%20Application%20Review%20Form_0.pdf, if they are the principal clinical provider without a physician partner, or they own and/or operate an independent practice. Physician assistants who only work with nurse practitioners, registered nurses, or other physician assistants need to have a practice agreement. Physician assistants with more than 4,000 clinical hours working in any other setting do not need to submit any forms.
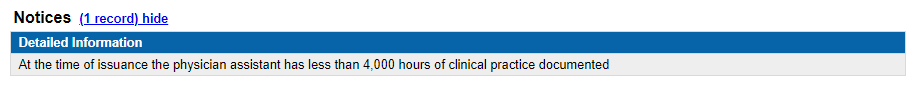
If you are a physician assistant and do not know if you have more than 4,000 clinical hours verified with the Board, you can go to our online search htthttp://www.pfr.maine.gov/ALMSOnline/ALMSQuery/SearchIndividual.aspx?Board=376, enter your name or license number and review the results. If there is a notice at the top of the screen that states, "At the time of issuance the physician assistant has less than 4,000 hours of clinical practice documented” you must submit a form prior to providing medical services in Maine. The notice looks like this:
If you are a physician assistant and believe you have 4,000 hours, proof of hours can be submitted to the Board at medicine.pfr@maine.gov. The easiest way to have your hours verified is to have your employer(s) submit a letter, on letterhead, that contains your start date, end date if applicable, full or part-time status, if you have been working in a clinical capacity, and the number of hours. For example,
Physician Assistant Smith has worked at Medical Office since January 1, 2019 in a full-time clinical capacity. During that time Ms. Smith has worked over 6,000 clinical hours.
Once the information has been verified the notice will be removed from the license.
If you have any questions, please contact our licensing staff.
Tracy Morrison
Licensure Specialist (207) 287-3602
tracy.a.morrison@maine.gov
Last Name A-L
Lisa Reny
Licensure Specialist (207) 287-3782
lisa.m.reny@maine.gov
Last Name M-Z
BOARD NEWS
Retiring Board Staff - Julie Best
After eight years of dedicated service to the Maine Board of Licensure in Medicine (“Board”), Julie Best, Complaint Coordinator, has retired from State service. The Board and Board staff will miss her.
Ms. Best was initially hired by the Board as its Consumer Assistance Specialist, the primary point of contact for the public regarding information about the Board’s complaint and investigative process. Within two years, Ms. Best was promoted into the newly created Complaint Coordinator position at the Board. In that capacity, Ms. Best supervised the Board’s Investigative Secretary and Consumer Assistance Specialist and assumed overall responsibility for the investigation of complaints and the monitoring of licensee compliance with Board Decision & Orders and Consent Agreements. Ms. Best was recognized for her organizational and professional communication skills by Board staff and others, including expert reviewers, the staff of the MPHP, and attorneys for licensees. Her intelligence, diligence, work ethic, team centered approach, and extremely positive attitude made her an effective and respected leader and example for Board staff. Ms. Best supported her staff to the utmost.
The Board and Board staff deeply thank Ms. Best for her professionalism and service, and her significant contributions toward the Board’s mission of protecting the public.
Editor-in-Chief David Nyberg, Ph.D. Graphic Design Ann Casady